The Potential of Optogenetics
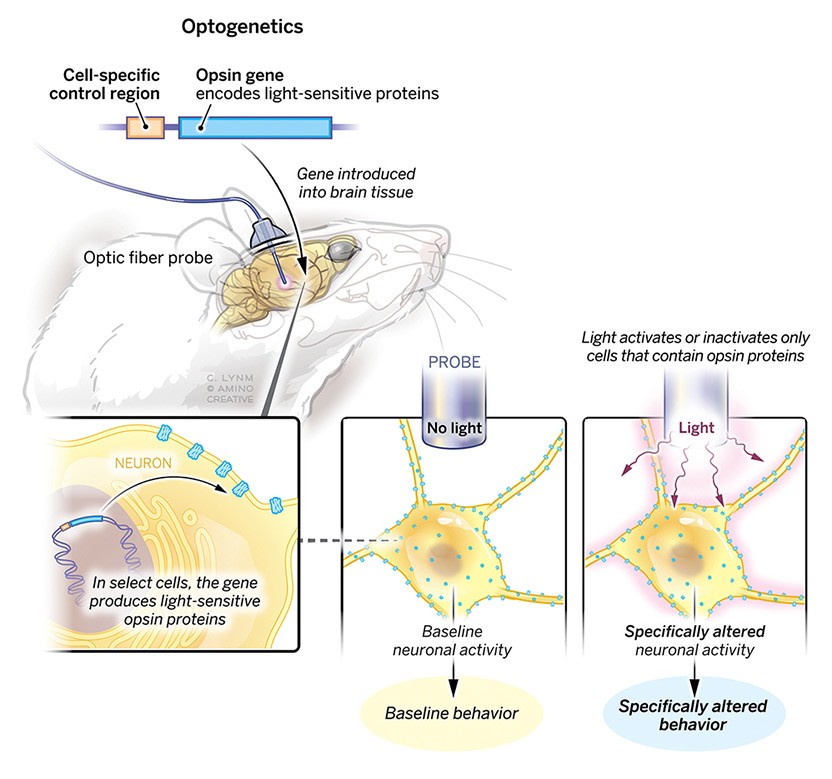
More than a decade ago, I had learned about an exciting new research technique called optogenetics. Back then, it was (and still is) largely considered a research tool. In essence, it’s a new(ish) way of activating genes with light. More importantly, it has the capability to regulate specific neurons. From a research standpoint, this is a breakthrough as existing techniques (e.g., eletrophysiology) have limitations. But the exiting part is this could become a new therapeutic modality, maybe.
Current tools for treating mental and behavioral disorders can be difficult to prescribe (e.g., SSRI non-responders) and manage (e.g., dose titration). Lots of drugs exist to treat disorders such as depression, anxiety, Schizophrenia, etc, but leave a lot to be desired – side effects, non-responders to certain medications and drug tolerance – all known issues.
Small molecule drugs hit many different receptors, at varying levels of specificity, so-called ‘dirty’ drugs. Sometimes it’s beneficial but often it’s not. Other interventions like transcranial magnetic stimulation or deep brain stimulation are marginally effective but entirely non-specific.

Because optogenetic approaches are capable of regulating specific clusters of neurons, it really does open the door to thinking about treating mental disorders in a new light. What if you could specifically activate cells within the substantia nigra, preventing neurodegeneration, for early-stage Parkinson’s Disease patients?
2021 Albert Lasker Basic Medical Research Award
You may have heard of the Lasker Award but if not, it’s kind of your film winning a Screen Actor’s Guild award before an Oscar. In the last 20 years, 32 Lasker Awardees have become Nobel laureates. Not a guarantee, but a pretty good bet.
Karl Deisseroth (Stanford), Peter Hegemann (Humboldt University of Berlin) and Dieter Oesterhelt (Max Planck Institute) were collectively honored with the 2021 award for “Light-sensitive microbial proteins and optogenetics”. Karl Deisseroth’s lab made a big contribution in 2007, where they demonstrated you could command the behavior in rats using a gene delivery system, light-sensitive gene and optical probe (see below).
But wait, it gets even better.
Translating Optogentics
Last year, Deisseroth’s group published a report demonstrating they could do this non-invasively (admittedly only up to 7mm), without the need for the intracranial probe seen above (Chen et al. (2021). This is more feasible in mice, due to their relative size; but does demonstrate working toward a significant challenge in this type of phototherapy (that is, light penetration limitations). A challenge but given it’s potential could be overcome in humans with new medical devices (i.e. light-delivering catheter). Snake a catheter through a blood vessel to your area of interest, then shine.
Another group in Germany demonstrated the use of optogenetics in a blind patient with Retinitis pigmentosa, a rare disorder where rod photoreceptors are lost. In this work, the group demonstrated they could partially restore vision by activating optogenetically transduced retinal cells (Sahel et al. (2021). This was a great proof-of-concept as ophthalmic indications are perfect for this type of thing.
I’m very interested in seeing more work on this, and am cautiously optimistic. The field has come a long way and hopefully more work will demonstrate optogenetic’s potential as a therapy. Stay tuned.
References
Chen, Ritchie, Felicity Gore, Quynh-Anh Nguyen, Charu Ramakrishnan, Sneha Patel, Soo Hyun Kim, Misha Raffiee, et al. 2021. “Deep Brain Optogenetics Without Intracranial Surgery.” Nat. Biotechnol. 39 (2): 161–64. https://doi.org/10.1038/s41587-020-0679-9.
Sahel, José-Alain, Elise Boulanger-Scemama, Chloé Pagot, Angelo Arleo, Francesco Galluppi, Joseph N Martel, Simona Degli Esposti, et al. 2021. “Partial Recovery of Visual Function in a Blind Patient After Optogenetic Therapy.” Nat. Med. 27 (7): 1223–29. https://doi.org/10.1038/s41591-021-01351-4.